Exposomics for Better Environmental Health
Why in the news?
On June 5, 2025, World Environment Day gave global attention to the question of plastic pollution. In India, observation came with considerable pressure on understanding the burden of extensive environmental disease. Dean (research) at the Shri Ramchandra Institute of Higher Education and Research. Kalpana Balakrishnan emphasised a large scientific border – the exposomics field. How this new science changes chemical, physical, biological and social risks throughout life promises to change our understanding. At a time when India has about a quarter of the burden of global environmental disease, exposomics can be a game changer for integrated evaluation of environmental health and policy formulation.
Background: Environmental health and global references in India
- Environmental risk factors such as air and water pollution, toxic chemical risk and inadequate hygiene are the most important contributors to the disease worldwide.
- The World Health Organisation (WHO) began determining the environmental impact of the disease in 2000 and has refined the process since the Global Burden (GBD) study.
- In its 2021 cycle, it was found that the risk factor for the environment and commercial (OEH) was responsible for 12.8 million deaths globally and 14.4% of all DALYs (disabled life years).
India faces an external challenge:
- More than 3 million deaths and 100 million DALYs are attributed to OEH risk.
- Environmental risk is responsible for more than 50% of non-infectious disease burden, such as heart disease, stroke, lung cancer and chronic kidney disease.
- Lead exposure for children under five has serious developmental damage, contributing 20% of 154 million lost IQ points, or 20% of the global total.
Features: What is Exposomics?
From Genome to Exposome
The sequencing of the Human Genome Project (1990–2003) revolutionised our understanding of genetics. Yet, it became clear that genes alone cannot explain many common diseases. For example, genetics accounts for less than half of heart disease risk.
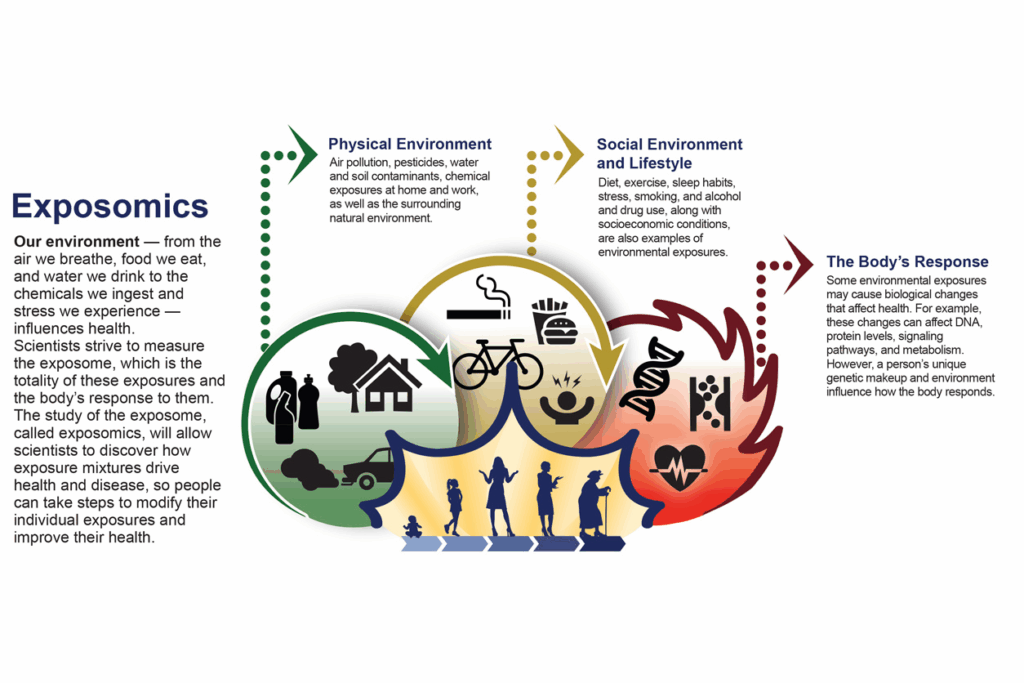
This led to the birth of exposomics, the comprehensive study of all environmental exposures (external and internal) throughout a person’s lifetime and their impact on health. While the genome is fixed, the exposome is dynamic and reflects a person’s interaction with their environment.
Components of the Human Exposome
- The exposome includes three domains:
- General external exposures (climate, pollution, socioeconomic conditions)
- Specific external exposures (diet, infections, lifestyle, drugs, radiation)
- Internal exposures (metabolism, inflammation, gut microbiota, oxidative stress)
- By capturing how these exposures interact with genetic, physiological, and psychosocial factors, exposomics offers a life-course perspective on disease development.
Technologies Enabling Exposomics
- The field relies on a suite of cutting-edge interdisciplinary technologies:
- Sensor-based personal monitoring: Wearable devices that track real-time exposure to pollutants.
- Untargeted chemical analysis: Using mass spectrometry to analyse thousands of environmental chemicals in biological samples.
- Organs-on-a-chip: Micro-physiological systems that mimic human organs to test responses to chemicals.
- Big data and AI: Integration and analysis of vast datasets to identify exposure-disease linkages (Exposome-Wide Association Studies or EWAS).
Challenges: Why Current Approaches Are Insufficient
Fragmented Policy and Data Silos
India’s environmental health management remains fractured across ministries and sectors — health, environment, water, agriculture, and urban development. This results in disjointed data collection, poor surveillance, and inconsistent regulation.Moreover, human exposure data is limited to a narrow range of factors like PM2.5 or arsenic in water.
Large data gaps exist in:
- Noise pollution
- Heavy metals beyond lead
- Endocrine-disrupting chemicals
- Microplastics
- Compound exposures and mixture effects
Incomplete Risk Estimations
Current GBD estimates under-report environmental risks because:
- Only ~11 risk categories are included due to a lack of exposure data.
Risk estimation models usually evaluate single exposures, ignoring the cumulative and interacting effects of multiple hazards over a lifetime. - Interactions with genetics, diet, stress, behaviour, and socio-economic status are insufficiently modelled.
This hampers the prioritisation of preventive strategies and obscures health inequities, especially in vulnerable populations.
Climate Change Multipliers
Environmental exposures are being magnified by climate change. Examples include:
- Heatwaves intensifying the health impacts of air pollution
- Flooding is increasing disease transmission.
- Crop failures affecting nutrition
- Wildfires releasing toxins
Climate-sensitive risks often co-occur and interact, creating compound events. These synergistic hazards are hard to quantify with existing tools.
Infrastructure and Institutional Barriers
India lacks a centralised exposomics initiative or a dedicated national centre for environmental health research. Additionally:
- Surveillance systems are weak or absent in many states.
- Public health laboratories are not equipped for exposomic monitoring.
- There is a severe shortage of trained personnel, interdisciplinary researchers, and funding.
Way Forward: Operationalising Exposomics in India
Establish a National Exposome Program
India should launch a National Human Exposome Project under the joint leadership of the Ministry of Health, the Ministry of Environment, and DST/DBT. Key priorities would include:
- Establishing regional centres of excellence
- Creating a national exposome database
- Linking environmental and health surveillance data
- Encouraging public-private partnerships for technology development
- Integrate Exposomics in Public Health Planning
Exposomics should inform the design of:
- Disease forecasting models
- Health impact assessments (HIA)
- Targeted interventions for vulnerable populations
- Urban planning, sanitation, and waste management policies
- It must also feed into precision public health, where interventions are customised by area, exposure, and population subgroup.
- Build Capacity and Infrastructure
Strategic investments are required in:
- Wearable monitoring and remote sensing technologies
- AI-enabled analytics and bioinformatics
- Interoperable data repositories
- Human biomonitoring labs with high-throughput capability
- India must also create multi-disciplinary educational programs combining public health, environmental science, data science, and toxicology.
Harmonise Regulations and Data Sharing
- Legal and policy reforms are essential to:
- Standardise environmental monitoring protocols
- Mandate real-time emissions and pollution disclosures
- Enable data sharing across ministries and with research institutions
- Encourage citizen science through participatory monitoring
Mobilise Communities and Youth
- Public awareness about environmental health is still low. National campaigns should:
- Promote individual-level behaviour change (e.g. reducing plastic use, avoiding open burning)
- Involve schools, colleges, and RWAs in participatory exposomic projects
- Leverage platforms like Poshan Abhiyan, Swachh Bharat Mission, and Ayushman Bharat for integration.
Case Study: Exposing capacity in handling diabetes and air pollution
- A fresh Lancet study showed how air pollution contributes significantly to diabetes. In Indian cities such as Delhi and Kanpur, where the level of PM2.5 is chronically high, researchers can perform exposure research:
- Track the first biomarker in the exposed population
- Determine the amount of cumulative risk from traffic, cook smoke and commercial sources
- Difference between genetic and environmental contribution
- Inform urban plans for urban health.
- Such evidence-based policy settings can reduce health costs and the incidence of the disease.
Conclusions
India’s growing environmental disease burden requires a paradigm shift for general, life-based environmental health strategies due to fragmented intervention. Exposic provides a revolutionary framework for understanding and addressing exposure, complicated and cumulative risks hidden by Indians, from the fetus to the elderly. The Human Genome Project changed the material, and now the Human Exposure Project can change public health. While we are at the intersection of environmental crisis and health emergency conditions, hugging is not just a time – this is necessary.
MAINS PRACTICE QUESTION
Questions: “The concept of exposures marks a paradigm change in understanding the complex relationship between environment and health. Seriously, check how exposures can change environmental health policy in India. Discuss researchers, infrastructure and challenges in implementing an exposure -based public health structure.”
PRELIMS PRACTICE QUESTION
Question .Consider the following statements regarding Exposomics:
- Exposomics examines the impact of only physical and chemical environmental exposures on human health over a lifespan.
- The exposome includes internal biological responses such as oxidative stress and inflammation.
- Exposomics research aims to replace genome-wide association studies (GWAS) with exposure-wide association studies (EWAS).
- In India, exposomic data is already integrated into the Global Burden of Disease (GBD) estimations.
Which of the statements given above is/are correct?
A. 2 only
B. 2 and 3 only
C. 1 and 4 only
D. 1, 3 and 4 only
Correct Answer: A. 2 only
Explanation:
- Statement 4 is incorrect: Exposomic data is not yet integrated into the GBD due to a lack of widespread human exposure data in India.
- Statement 1 is incorrect: Exposomics includes physical, chemical, biological, and psycho-social exposures, not just physical and chemical ones.
- Statement 2 is correct: The exposome includes internal exposures such as oxidative stress, inflammation, and gut microbiota.
- Statement 3 is incorrect: EWAS are intended to complement GWAS, not replace them.